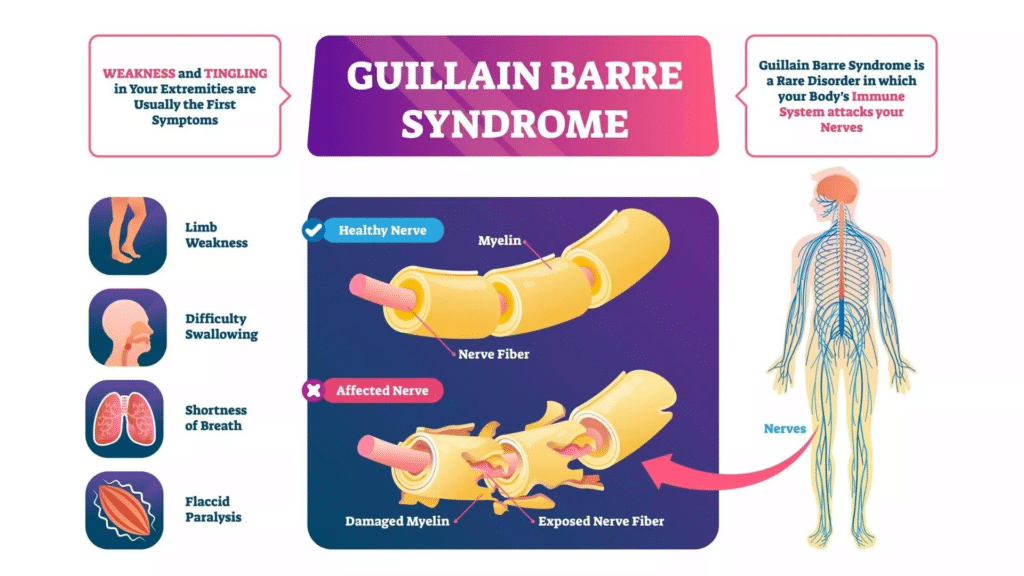
Guillain-Barré Syndrome (GBS), pronounced Ghee-yan Bah-ray, is a rare and serious autoimmune neurological disorder where the body’s immune system mistakenly attacks the peripheral nervous system. This network of nerves carries signals between the brain, spinal cord, and the rest of the body. The condition typically manifests suddenly, escalating in severity over hours, days, or weeks. While some cases are mild and marked by brief weakness, others can lead to near-total paralysis, interfering with vital functions such as breathing, blood pressure, and heart rate. Fortunately, most individuals recover from even the most severe cases, although some may experience lingering symptoms like weakness or numbness.
Symptoms of Guillain-Barré Syndrome
GBS symptoms can vary widely but typically include:
1. Weakness:
- Rapid onset of muscle weakness, often starting in the feet and legs before progressing upward.
- In some cases, weakness may begin in the face and move downward.
- Difficulty climbing stairs, walking, or performing everyday tasks.
2. Sensation Changes:
- Tingling or “pins and needles” sensations, often in the hands or feet.
- Deep muscular pain, particularly in the back or legs.
- Unexplained sensations like crawling insects under the skin (formications).
3. Additional Symptoms:
- Difficulty with eye movement, vision, swallowing, speaking, or chewing.
- Severe pain, particularly at night.
- Unsteadiness, coordination problems, or abnormal heart rate and blood pressure.
- Problems with digestion and bladder control.
Causes and Risk Factors
The exact cause of GBS remains unknown, but the disorder often follows a bacterial or viral infection. Common triggers include:
- Campylobacter jejuni infection (a leading cause of gastroenteritis).
- Viral infections such as Zika virus, Epstein-Barr virus, cytomegalovirus, or COVID-19.
- Recent surgeries.
- Rarely, vaccinations.
GBS can affect anyone, but it is more common in adults over 50 years of age. The condition is not contagious or hereditary but is classified as an autoimmune disease, where the immune system mistakenly attacks healthy nerve cells, often mistaking them for invading bacteria or viruses.
Types of Guillain-Barré Syndrome
- Acute Inflammatory Demyelinating Polyradiculoneuropathy (AIDP): The most common form, involving damage to the myelin sheath surrounding nerve axons.
- Acute Motor Axonal Neuropathy (AMAN) and Acute Motor-Sensory Axonal Neuropathy (AMSAN): These types involve direct damage to the axons themselves.
- Miller Fisher Syndrome (MFS): A rare variant affecting the cranial nerves, leading to issues with eye movement, balance, and coordination.
Diagnosing Guillain-Barré Syndrome
GBS can be challenging to diagnose due to its varied symptoms and overlap with other disorders. Common diagnostic approaches include:
- Medical History and Physical Exam: Doctors assess symptom onset, progression, and whether weakness affects both sides of the body.
- Nerve Conduction Velocity Test (NCV): Measures the speed of electrical signals along nerves, which are slowed in GBS due to nerve damage.
- Cerebrospinal Fluid Analysis: Analyzes spinal fluid for elevated protein levels and fewer immune cells, characteristic of GBS.
- Imaging: MRI scans may help rule out other causes of muscle weakness.
Treatment Options
Although there is no cure for GBS, timely interventions can reduce severity and improve recovery outcomes. Common treatments include:
- Plasma Exchange (Plasmapheresis):
- Removes harmful antibodies from the blood plasma, reducing nerve damage.
- Intravenous Immunoglobulin Therapy (IVIg):
- Involves injecting immunoglobulins from healthy donors to neutralize harmful antibodies and reduce inflammation.
- Supportive Care:
- Close monitoring in an intensive care unit (ICU) for breathing difficulties, heart rate irregularities, and other complications.
- Mechanical ventilation for severe respiratory issues.
- Physical therapy to maintain muscle flexibility and strength during recovery.
- Rehabilitation:
- Physical, occupational, and vocational therapies help patients regain strength, mobility, and independence.
Latest Research and Updates
Research into GBS is ongoing, focusing on understanding its causes, improving treatments, and identifying genetic risk factors. Some key areas of progress include:
- Immune System Studies: Researchers are investigating how certain bacterial and viral proteins may trigger autoimmune attacks on the nervous system.
- Genetic Links: Studies are exploring genetic variations that could increase susceptibility to GBS.
- Enhanced Therapies: Efforts are underway to improve IVIg and develop new treatments that target inflammation and prevent nerve damage more effectively.
- Animal Models: Mouse models are being used to study autoimmune responses and identify specific peripheral nervous system proteins at risk.
Living with Guillain-Barré Syndrome
While most people recover fully from GBS, the journey can be long and challenging. Recovery may take weeks to years, and some individuals experience long-term effects such as:
- Persistent weakness or fatigue.
- Residual numbness or pain.
- Emotional challenges due to sudden paralysis and dependence on others.
Support groups and mental health counseling can play a crucial role in helping individuals cope with these challenges. Participation in clinical trials also offers an opportunity to contribute to research and improve care for future patients.
Guillain-Barré Syndrome, though rare, is a serious and potentially life-altering condition. With advancements in research and treatment, the prognosis for individuals with GBS continues to improve. Early diagnosis, timely treatment, and comprehensive rehabilitation are key to recovery, offering hope and resilience to those affected by this challenging disorder. For anyone experiencing symptoms, prompt medical attention is crucial to ensure the best possible outcome.


